Nipah Virus India 2026: Symptoms, Prevention, and Latest Health Alerts in West Bengal
The Return of the Nipah Virus: A Comprehensive Guide to India’s 2026 Outbreak
In the second week of January 2026, India’s health landscape was hit by a familiar but deadly name: the Nipah Virus. The National Institute of Virology (NIV), Pune, confirmed the presence of the virus in healthcare workers in the North 24 Parganas district of West Bengal. As the nation grapples with this re-emergence, understanding the nature of this pathogen, its symptoms, and the necessary precautions is vital for public safety.
1. The Current Situation (January 2026)
The 2026 outbreak is particularly significant because it marks the return of Nipah to West Bengal after 19 years (the last major outbreaks were in Siliguri in 2001 and Nadia in 2007). Two healthcare workers in Barasat initially tested positive, with one reportedly slipping into a coma and another on ventilator support.
Following these cases, the Union Health Ministry deployed a National Joint Outbreak Response Team (NJORT) to assist the state government in contact tracing and containment. An alert has been sounded in Jharkhand, Bihar, and Odisha, as these states share borders and see high population movement with West Bengal.
2. What is the Nipah Virus?
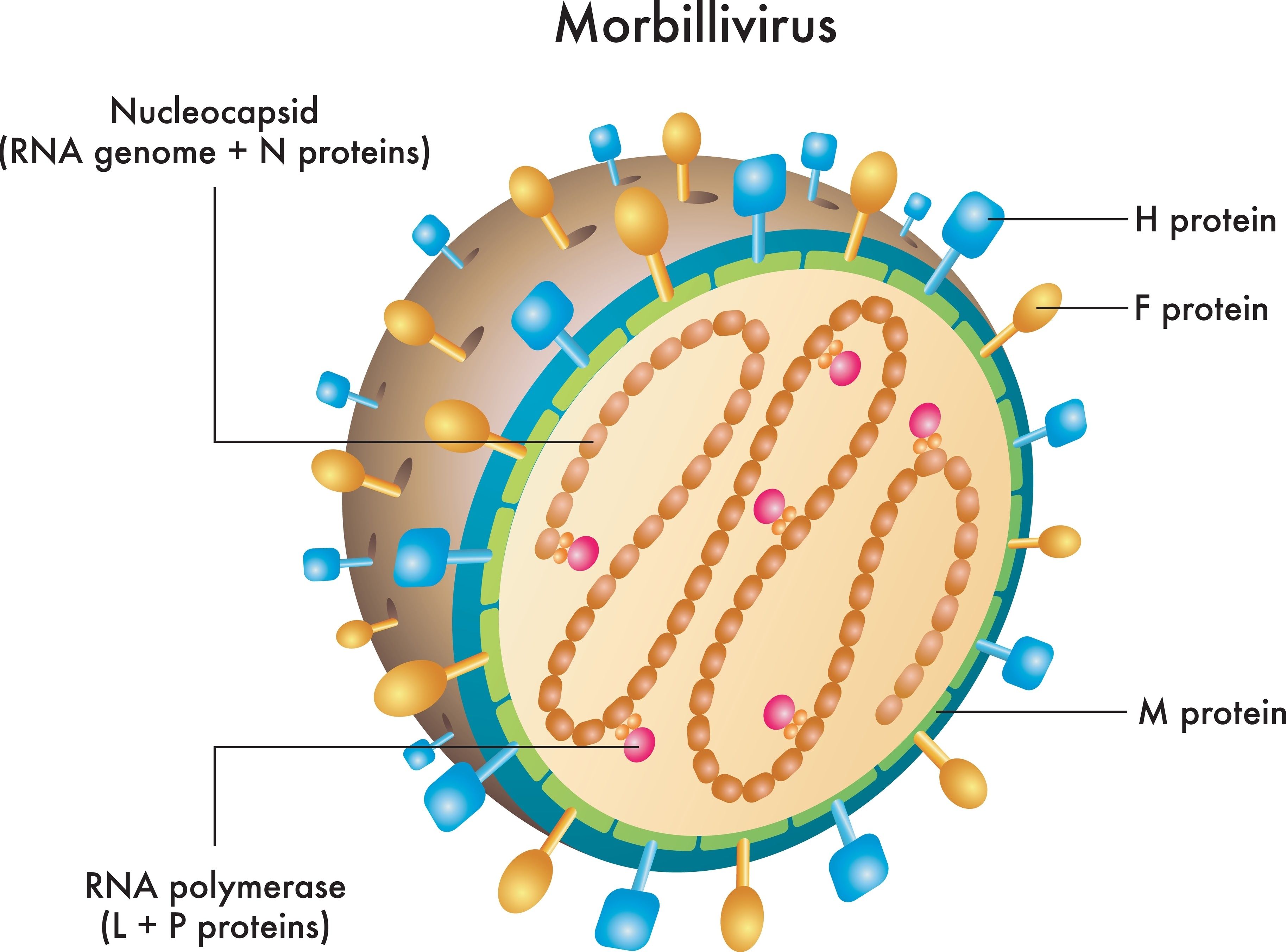
Nipah Virus (NiV) is a zoonotic virus, meaning it is transmitted from animals to humans. It belongs to the Henipavirus genus and is considered one of the deadliest pathogens known to man, with a Case Fatality Rate (CFR) ranging from 40% to 75%.
The natural hosts of the Nipah virus are fruit bats (specifically those of the Pteropodidae family, Pteropus genus). These bats carry the virus without getting sick themselves. They often shed the virus through their saliva, urine, and excreta.
3. How the Virus Spreads (Transmission)
Understanding how Nipah spreads is the first step toward prevention. There are three primary routes of infection:
A. Animal-to-Human Transmission
This occurs through direct contact with infected animals (bats or pigs) or their body fluids. In many Indian outbreaks, the primary source has been the consumption of fruits (like mangoes or guavas) that have been partially eaten or contaminated by bat saliva.
B. Contaminated Food
Drinking raw date palm sap is a major risk factor. Bats often visit date palm trees at night to drink the sap, contaminating the collection pots with their urine or saliva. When humans consume this raw "toddy" or juice, the virus enters the body.
C. Human-to-Human Transmission
Unlike many other zoonotic viruses, Nipah can spread between people. This usually happens in a "close contact" setting:
Caregivers: Family members looking after an infected person.
Healthcare Settings: Nurses and doctors (as seen in the current 2026 Bengal cases) who handle patients without adequate Personal Protective Equipment (PPE).
Bodily Fluids: Spread through respiratory droplets, blood, urine, or saliva.
4. Symptoms and Clinical Progression
The incubation period (time from infection to onset of symptoms) usually ranges from 4 to 14 days, though it can extend up to 45 days in rare cases.
Initial Phase (Flu-like)
The disease often starts with non-specific symptoms that can be mistaken for a common cold or flu:
High fever and chills
Severe headache
Muscle pain (myalgia)
Sore throat and persistent cough
Nausea and vomiting
Severe Phase (Neurological and Respiratory)
As the virus progresses, it attacks the brain (encephalitis) and the lungs:
Acute Respiratory Distress: Severe difficulty in breathing.
Encephalitis: Inflammation of the brain leading to drowsiness, disorientation, and mental confusion.
Seizures: Abnormal electrical activity in the brain.
Coma: In severe cases, patients can slip into a coma within 24 to 48 hours of developing neurological symptoms.
5. Why Nipah is Especially Dangerous
Unlike COVID-19, which spreads rapidly but has a lower mortality rate, Nipah spreads less easily but is far more lethal.
No Vaccine: As of January 2026, there is no approved vaccine for humans or animals.
No Specific Treatment: There is no specific antiviral drug. Treatment is purely "supportive care," which involves managing symptoms and keeping the patient hydrated and ventilated.
High Mortality: The high death rate makes it a "Priority Pathogen" for the World Health Organization (WHO).
6. How to Protect Yourself: Prevention and Safety
Prevention is the only shield against Nipah. Following these guidelines can significantly reduce your risk:
Dietary Precautions
Avoid Fallen Fruits: Never eat fruits found on the ground or those with visible bite marks or scratches.
Wash Fruits Thoroughly: Peel fruits before eating and wash them under running water.
Say No to Raw Date Palm Sap: Ensure that any date palm juice is boiled thoroughly before consumption. Avoid "toddy" in areas where bat activity is high.
Personal Hygiene
Frequent Handwashing: Use soap and water regularly, especially after visiting public places or hospitals.
Use Masks: While Nipah is not as airborne as the flu, wearing a mask in crowded areas or healthcare settings is a good safeguard.
Avoid Bat Habitats: Stay away from areas where fruit bats congregate, such as old wells, fruit orchards, or abandoned buildings.
Caregiving and Hospital Safety
Maintain Distance: If someone in your community has a fever with confusion/disorientation, maintain a safe distance and report it to health authorities immediately.
Strict PPE: Healthcare workers must use N95 masks, gloves, and gowns when treating suspected cases.
Safe Burial: The bodies of those who succumb to Nipah remain infectious. Burial or cremation must be handled by trained professionals following strict protocols.
7. Government Response and Public Responsibility
The Indian government has activated the Integrated Disease Surveillance Programme (IDSP) to monitor fever clusters across the country.
What should you do?
Don't Panic: Nipah outbreaks are usually localized. Panic leads to the clogging of healthcare systems.
Verify Information: Avoid spreading "WhatsApp forwards" about new cures. Follow only the Ministry of Health and Family Welfare (MoHFW) or WHO advisories.
Early Reporting: If you or someone you know has recently traveled to an affected area and develops a high fever, seek medical help immediately. Mention your travel history to the doctor.
8. Conclusion
The 2026 Nipah alert in India is a stark reminder of our vulnerability to zoonotic diseases. While the high mortality rate of the virus is frightening, the history of successful containment in Kerala shows that rapid isolation, strict hygiene, and public awareness can stop the virus in its tracks. By staying informed and practicing basic food safety, we can navigate this health challenge together.

Comments 0